Moms often experience fatigue, pain and difficulty breastfeeding during this period, causing many to reduce the frequency of breastfeeding. Howevever, the opposite is true - breastfeeding more often usually helps get rid of the infection, and the baby is still safe while feeding. Mastitis is a serious discomfort, but can be easily treated.
Common Causes of Mastitis
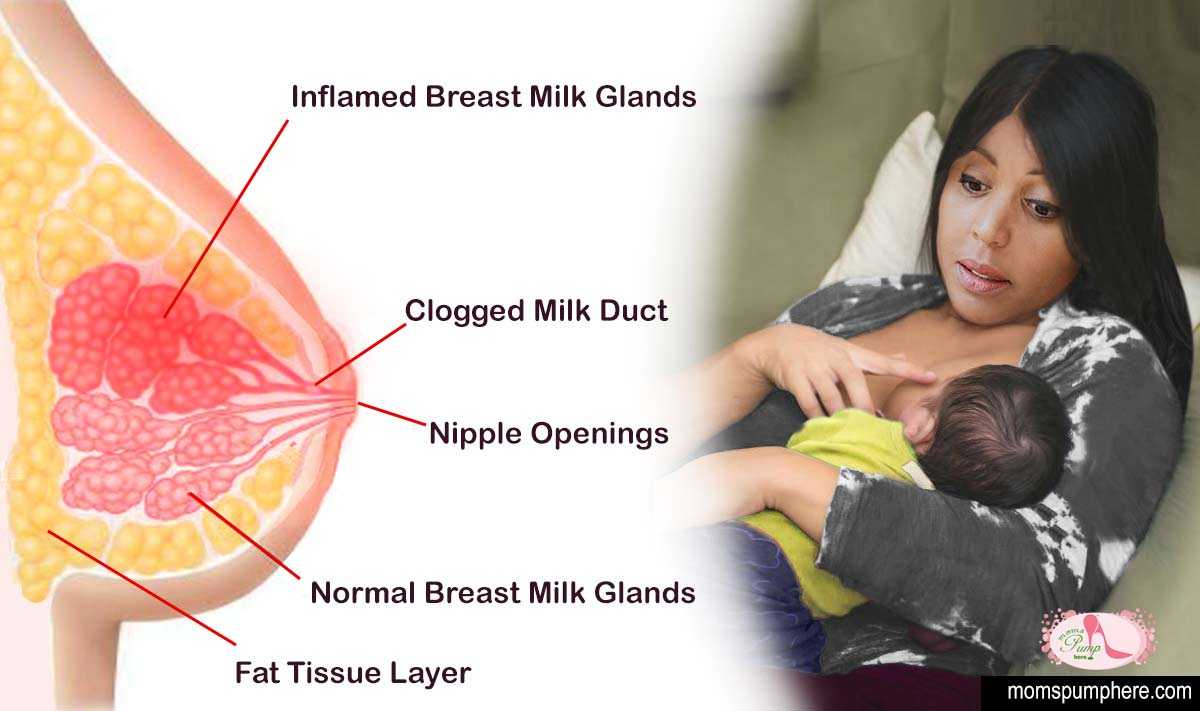
Mastitis most often happens when bacteria enter the breast through a cracked or sore nipple due to engorgement (swelling of the breast from over-production of breast milk), plugged milk ducts, or milk that remains in the breast after a feeding (milk stasis).
Extended periods between a regular nursing schedule or not fully emptying your breast through feeding or pumping increase the chances of getting mastitis. Proper latching and rotating your breastfeeding techniques helps to empty your breasts and prevent cracked sore nipples.
Common Symptoms of Mastitis
First hints of mastitis usually begin as a painful spot in one breast. The external area around that spot may get visibly red, warm in sensation , or both. Fever, chills, and body aches may also accompany the initial symptons. Greater signs your mastitis has gotten worse include pain and swelling of lymph nodes in your armpit near the affected breast, heart rate speeds up, and flu-like symptoms worsen. A breast abscess (painful lump), is usually the final symptom of mastitis if left untreated in early stages.
Will you get mastitis?
The odds you'll get mastitis increase if:
Breastfeeding mothers are very susceptable to mastitis especially the first two months of nursing when the baby's feeding pattern is not regular. After that, the chances of getting mastitis are lowered when a regular feeding pattern is created.
How do doctors diagnose mastitis?
Mastitis is generally easy to diagnose following the CDC (Center for Disease Control) criteria #3 for breast abscess or mastitis in all of the following:
How to Treat Mastitis
Doctors precscribe antibiotics as the general treatment for mastitis. Follow the prescribed directions directly as stated, and make sure the entire prescription of pills are used (This is VERY important). The baby is safe from the antibiotics in your body. If you see no improved results after using the antibiotics, your physician will test a sample of your breast milk at a lab to identify the specific bacteria causing your mastitis. They (your doctor) can then recommend a more specific antibiotic treatment.
You can help yourself feel better by getting more rest, drinking more fluids, and using warm or cold packs on your painful breast.
Before breastfeeding your baby, place a warm, wet washcloth over the affected breast for about 15 minutes. Try this at least 3 times a day. This increases milk flow in the breast. Massaging the affected breast may also increase milk flow.
You can safely take acetaminophen (such as Tylenol) for pain or a fever. You can take ibuprofen (such as Advil) along with acetaminophen to reduce inflammation. Be safe with medicines. Read and follow all instructions on the label.
Breastfeeding from your affected breast is safe for your baby. If starting with the affected breast is too painful, try feeding your baby with your healthy breast first. Then, after your milk is flowing, breastfeed from the affected breast. If your nipples are too cracked and painful to breastfeed from that breast, hand express or use a breast pump to empty the breast of milk. Try this each time that you cannot breastfeed.
You should see a lactation consultant for best help in dealing with mastitis. They're usually equipped to help you breastfeed more effectively with less pain. The Lactation Consultant usually a nurse who specialize in issues related to breastfeeding can give advice and offer solutions to prevent future occurances of mastitis. LC's often recommend you change positions and make sure your baby is latching on properly.
Be sure to get treatment for mastitis. Delaying treatment can lead to a breast abscess, which can be harder to treat.
Always consult a doctor or licensed medical professional for additional and final advice.
References:
cdc.gov
webmd.com